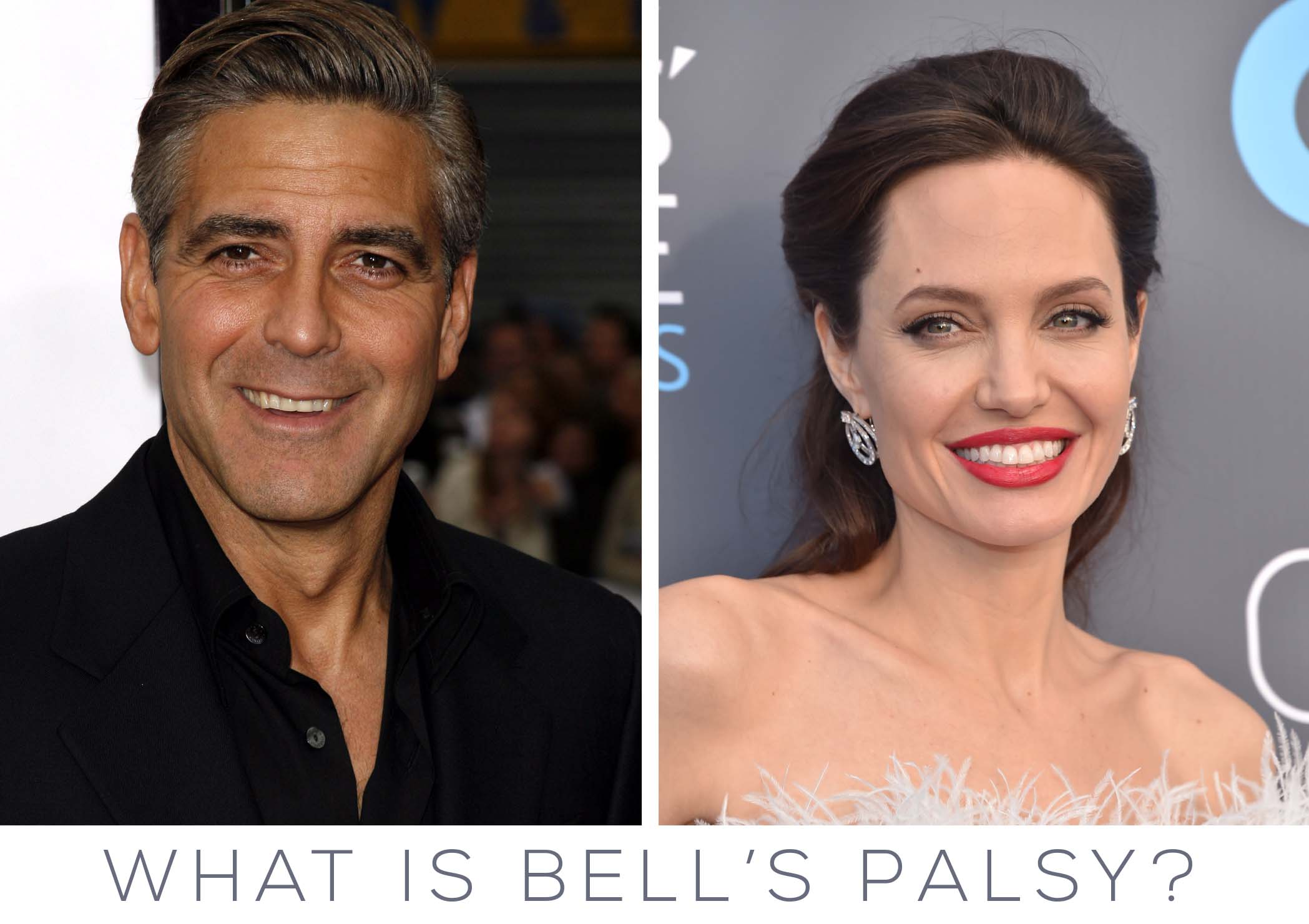
Earlier last year, Oscar award winning actress, Angelina Jolie came forward with a surprising diagnosis of Bell’s Palsy, a form of temporary facial nerve paralysis. At the time, this was a condition few Americans had heard of, but soon other A-List celebrities, like George Clooney, followed suit and came forward to discuss their battles with Bell’s Palsy. What exactly is this condition? Why does it happen? As it turns out, this condition, and other forms a facial nerve paralysis are more common than you may think.
The National Institute of Neurological Disorders and Stroke defines Bell’s Palsy as damage or trauma to the facial nerve (the seventh facial nerve in the case of Bell’s Palsy), which, in turn, causes a disruption of the nerve signal at its origin at the brain stem to the muscles of the sides of the face. The result? The patients’ ability to move or express their face may be dramatically impacted.
“A patient experiencing Bell’s Palsy may have difficulty with expressions such as raising their eyebrows, blinking, and smiling,” shares Dr. Garrett Griffin, a Facial Plastic Surgeon and facial paralysis expert at Midwest Facial Plastic Surgery. “In some cases, their sense of taste may even be affected,” he adds. He continues, “Although both sides of the face may be affected, it is most common to see it only affect one side.”
The cause of Bell’s Palsy is not completely known, though it is most likely caused by reactivation of the Herpes Simplex Virus within the facial nerve. The nerve swells and gets trapped within its bony canal at the base of the skull, resulting in loss of blood supply to the nerve and reduced or absent facial movement. Most patients (85%) with Bell’s Palsy recover with no sequelae but 15% will be left with facial spasm or uncontrolled facial movement called synkinesis. Bell’s Palsy never causes permanent facial weakness…if the weakness extends beyond 6 months a different cause must be sought out.
Bell’s Palsy is the most common cause of facial weakness but there are many possible causes of facial paralysis.
- Infection or inflammation of the facial nerve
- Head trauma
- Head or neck tumor
- Stroke or blood pressure disorders
- An error in fetal development or trauma during birth
- Accidental trauma to the nerve during a car accident or fall. Sometimes this is because there is a fracture of the bone at the skull base where the nerve enters the face
- Autoimmune diseases including Wegener’s disease
- Neurologic diseases including multiple sclerosis
- Other infections including Lyme disease or shingles of the face
- Chronic ear problems like cholesteatoma
Facial paralysis can come on suddenly (in the case of Bell’s Palsy), or happen gradually over a period of months (in the case of a head or neck tumor). Depending on the cause, the paralysis might last for a short or extended period of time. In either circumstance, the condition can be devastating for patients and affect various aspects of their lives. Fortunately, there are treatments available to improve these conditions.
Are there treatments for poor recovery after Bell’s Palsy, ie. for synkinesis?
Yes! Botulinum toxin (Botox) can be injected into the spastic and overactive muscles which can help people better control their facial movements and make them more comfortable. Patients can also work with a skilled occupational or physical therapist to learn stretches and biofeedback to improve facial control.
Are there treatments for complete facial paralysis?
Unlike Bell’s Palsy, some injuries to the facial nerve cannot recover. For example, if the nerve needs to be cut out for cancer, the nerve cannot spontaneously recover. In other instances, the nerve may be stretched and it can take up to 12 months to know if the nerve will be able to recover on its own or not. Fortunately, there are many reliable surgical treatments for chronic facial paralysis. The choice of treatment depends on how much time has passed since the injury and whether or not there is still a chance for spontaneous recovery.
“The surgical treatments that our clinic offers for facial nerve paralysis can basically be broken down into 5 categories,” advises Dr. Griffin.
1. Static procedures: Static procedures mean that they do not create facial movement. Likely the most common procedure performed for chronic facial paralysis is an upper lid gold or platinum weight. This is a static procedure where a small, sterile piece of gold or platinum is placed in the upper eyelid to help gravity close the eye during blink. Another common static procedure is aptly named a “static sling.” In this surgery, the paralyzed cheek is suspended in a more symmetric, elevated position.
2. Nerve grafts: When a portion of the nerve is removed by trauma or surgery, it can be replaced with a piece from a different nerve if both cut ends of the nerve can be identified.
3. Nerve substitutions (hypoglossal-facial nerve transfer or masseteric-facial nerve transfer): If the facial nerve is damaged or removed very close to the brain, a nerve graft is often not possible. However, it is possible to sew the nerve to the tongue (hypoglossal nerve) or a chewing nerve (masseteric nerve) to the stump of the facial nerve. Then, one can move the tongue or bite down in order to move the face.
4. Muscle substitutions (temporalis tendon transfer): When the muscles that move the face are paralyzed for 2 years or longer, they tend to shrink or atrophy and no longer function, even if you give them back nerve input. In these instances, you have to bring a new muscle into the face instead of a nerve. The most common and modern example of this technique is called temporalis tendon transfer. In this surgery, one of the chewing muscles (the temporalis muscle) is detached from the lower jaw and sewn to the corner of the mouth. Then, when the person bites down, it will create a smile on the paralyzed side of the face.
5. Cross-facial nerve graft and free muscle transfer: The only way to restore a completely emotional and spontaneous smile is to perform a 2-stage surgery called cross-facial nerve grafting with free muscle transfer. In the first stage, a nerve graft from the leg (sural nerve) is harvested and attached to a nerve branch that creates a smile on the normal side of the face. The nerve graft is tunneled across the upper lip and left near the corner of the mouth on the paralyzed side. After about 6 months, nerve fibers (axons) will grow across the nerve graft. At that point, the second stage is performed. A muscle from the leg (the gracilis muscle) is moved with its nerve and blood vessels to the paralyzed side of the face, and attached to blood vessels there so that the muscle will live. The nerve to the muscle is attached to the nerve graft from the first stage. Now, the brain can tell the good facial nerve, can tell the nerve graft, and can tell the muscle graft, to move when laughing or smiling. The entire gracilis flap process takes about 2-3 years and has a 20% failure rate in most large studies.
“I cannot stress enough the impact facial nerve paralysis may have on a patient,” says Dr. Griffin sadly. “Sufferers are usually incredibly self-conscious about their appearance and feel they can’t effectively communicate,” he continues, “it is so important for them to know that there are treatment options available to them and that they will be treated with the utmost respect, kindness and understanding at our clinic.”
Are you, or someone you know suffering from Facial Nerve Paralysis? If so, please do not hesitate to schedule a consultation with Dr. Garrett Griffin. Call (651) 632-9700